Step 01
Keep eating gluten
If you avoid or restrict gluten prior to testing for coeliac disease, your test results can be inaccurate.
If you have been avoiding gluten for more than around 6 weeks before testing, you will need to re-introduce gluten to the diet to ensure your test results are reliable and accurate. This is called a ‘gluten challenge’.
Step 02
Blood screening test
A blood test for coeliac disease (also called ‘coeliac serology’) is done to measure the level of certain antibodies (part of our bodies defence system). Your local GP can organise this for you.
The doctor will request either:
Transglutaminase-IgA (tTG-IgA) AND deamidated gliadin peptide-IgG (DGP-IgG) antibody tests
OR
Transglutaminase-IgA (tTG-IgA) antibody test AND the total IgA level
If your coeliac antibody level is above the normal range, this indicates you may have coeliac disease (the results of these blood tests on their own should not be used to diagnose coeliac disease). Do not start a gluten free diet yet, even if your blood test is positive (it is possible to have a positive blood test and not actually have coeliac disease). You need to see a specialist (a gastroenterologist) to confirm the diagnosis.
Step 03
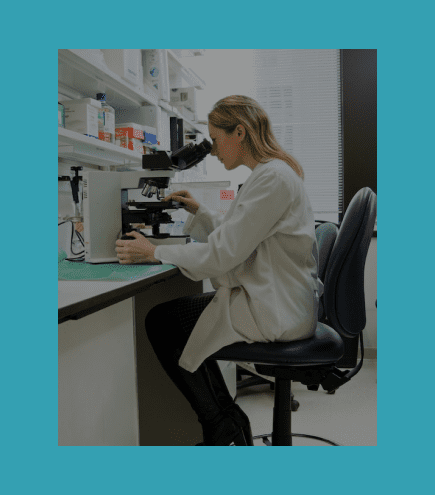
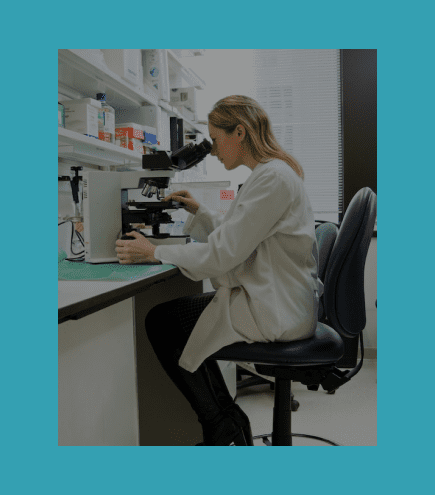
Small bowel biopsy
A diagnosis of coeliac disease is made by a gastroenterologist (a doctor who specialises in the gut).
Your gastroenterologist will perform a gastroscopy (also called an endoscopy) to collect tiny samples (biopsies) of the small bowel. A gastroscopy is a day procedure done under light sedation; while you are sedated, a ‘gastroscope’ (a thin flexible tube) is passed through your mouth and into your small bowel to allow the biopsies to be collected. The biopsies are examined under a microscope to confirm coeliac disease.
This procedure also helps to exclude other diagnoses that may be causing symptoms. Understanding the degree of small bowel damage is helpful for follow-up care.


Diagnosis in children
In some children a biopsy may not be necessary. Specific criteria will be assessed by your paediatric gastroenterologist (child gastroenterologist) when deciding whether a biopsy is needed.
Read moreGene testing (HLA genes)
The “coeliac gene test” tests for the main genes associated with coeliac disease: HLA-DQ2 and HLA-DQ8. At least one of these genes is necessary for coeliac disease to develop, but their presence alone does not mean the person has (or will ever get) coeliac disease.
This test is not always required but may be useful in certain situations, mainly as a way of excluding a diagnosis of coeliac disease. It can be useful when the diagnosis of coeliac disease is unclear. It is done by blood test or cheek (buccal) scraping and can be ordered through your local doctor.
A negative gene test is very helpful as it means coeliac disease can be excluded (you must have a coeliac gene to be able to get coeliac disease). A positive gene test indicates susceptibility to coeliac disease but does not diagnose coeliac disease. Approximately half of the general population is positive for the coeliac genes but only a small proportion will ever develop coeliac disease (most people with coeliac genes will never develop coeliac disease).
A gluten free diet should only be started after confirmation of coeliac disease by your specialist.
You do not need to be eating gluten for the gene test to be accurate. It can therefore be a useful first step of the gluten challenge process when people have removed gluten from their diet before testing. If the gene test is positive, then a gluten challenge followed by small bowel biopsy will be required to test for coeliac disease. However, a negative gene test rules out coeliac disease, allowing you and your doctor to explore other reasons for your symptoms.
Fact sheets
Testing and diagnosis of coeliac disease in children


Introducing gluten to a baby’s diet
Beware of unorthodox diagnosis techniques
It is common to come across inappropriate tests being promoted for the diagnosis of medical conditions, including food intolerances. These tests lack credible evidence, provide misleading results, can delay a correct diagnosis and lead to unnecessary and sometimes harmful treatments that don’t actually work. And as they are not rebated by Medicare, they are also at great expense to the individual. More information can be found in our ‘Unorthodox testing for coeliac disease‘ fact sheet.
Why should I be tested?
The gluten free diet is not for everyone and is not a ‘healthier’ way to eat. There are nutritional risks associated with following a restrictive diet which must be carefully managed. A gluten free diet is only recommended for those with coeliac disease or another medical need.
It is important to know what you have… this ensures that you are treating the right condition with the most appropriate treatment. By confirming a diagnosis of coeliac disease, you can be sure that your symptoms are not due to another condition that could be more sinister.
A clear diagnosis can help you stay motivated to stick to your gluten free diet and will also ensure you receive the necessary follow up to manage your coeliac disease.